Press Release

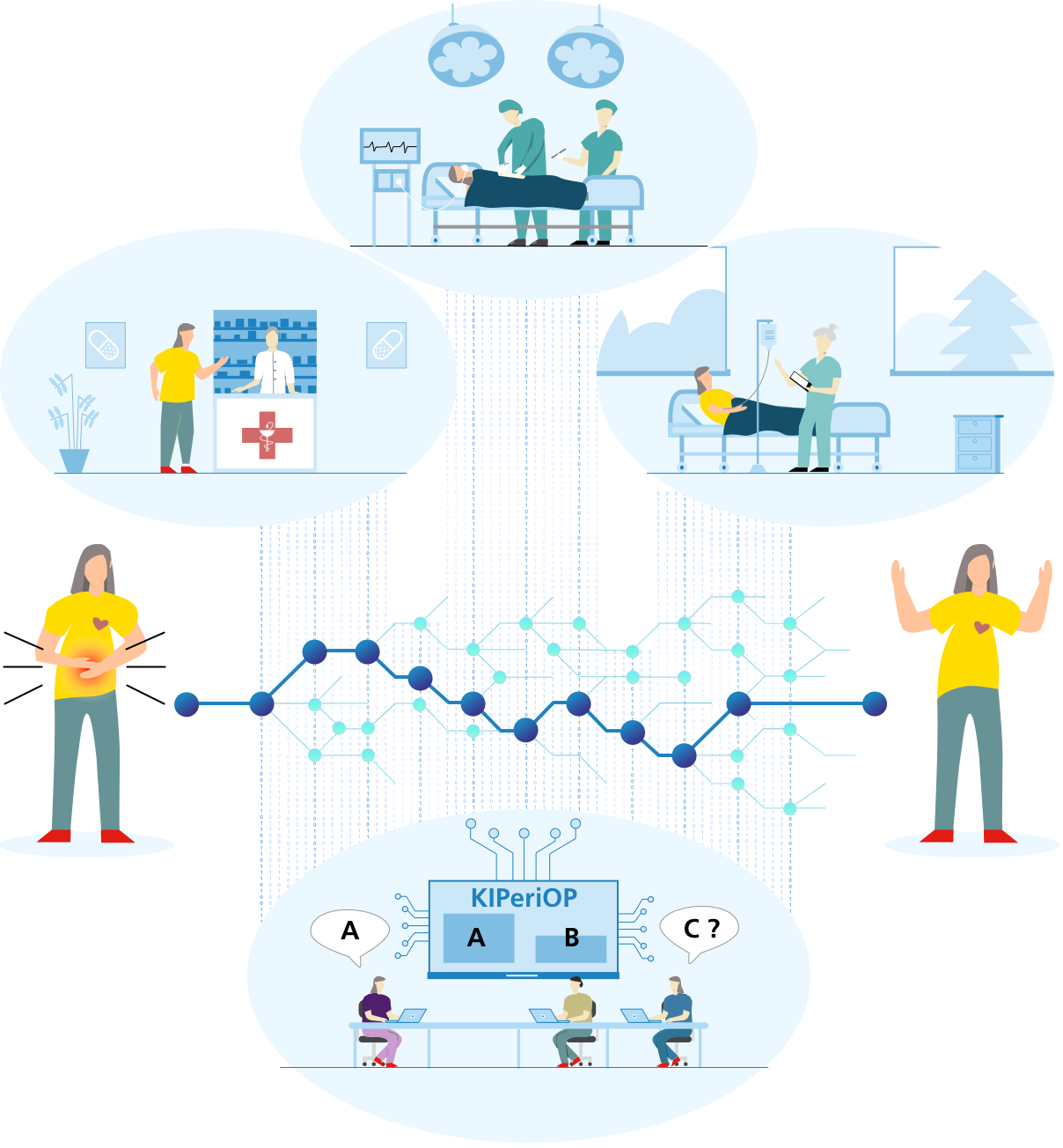
Complications can always occur during operations, sometimes resulting in death. A new project called KIPeriOP aims to minimize the risk of such complications. The project is based on digitized decision guidelines and self-learning algorithms intended to provide reliable risk assessment based on individual patient data. What is the probability that certain complications will occur, and how might they be avoided? The project is coordinated by Prof. Dr. Anja Hennemuth from the Fraunhofer Institute for Digital Medicine MEVIS and Prof. Dr. Patrick Meybohm from the University Hospital of Würzburg. Clinicians from the Asklepios Medical School GmbH, the University Hospital Frankfurt and the Charité – Universitätsmedizin Berlin are involved. They are working together with experts from the fields of AI, user guidance, ethics, and health economics.
More than 16 million operations are performed every year in Germany. Complications occur time and again, and sometimes lead to death. In Western industrialized nations, 0.4 to 0.8 percent of patients die during or following an operation. Hospitals often try to reduce this by accounting for possible risk factors. What are a patient’s accompanying diseases? What medications are being taken? What complications might arise, and how could these be minimized?
There are already guidelines to assist medical personnel during risk assessment. They list, for instance, the type and number of useful preliminary examinations. But in the real world, these guidelines aren’t always easy to apply. The guidelines are complex documents and employing them requires considering a wealth of information that is sometimes not easy to obtain.
Algorithms that assess risk
Here is where the KIPeriOP research project, carried out by an interdisciplinary consortium, comes into play. The goal is to develop a clinical decision support (CDS) system. Software developed by publisher Börm-Bruckmeyer will gather possible risk factors on a patient-specific and guideline-compliant basis, correlate them with each other, and deliver a risk assessment. How likely is it that a particular patient experiences serious complication during or after surgery? “Based on this risk assessment, clinicians can decide, for example, whether additional examinations are needed and what can be done to prepare the patient optimally for surgery,” explains Meybohm.
As much patient information as possible should be fed into the CDS system, including laboratory values, medication schedule, vital signs, and information about lifestyle habits. In addition to considering the guideline, KIPeriOP will employ artificial intelligence (AI) to analyze the digitally captured data. Learning algorithms will search out patterns and correlations that expose which groups of risk factors are likely to lead to which complications. With the help of AI, for example, it might be easier to recognize when a patient suffers from undiagnosed cardiac insufficiency and therefore an increased risk of surgery.
In the project, various AI methods will be tested to discover an optimal model. To work reliably, the algorithms must first be trained by feeding them with many data sets from real preliminary examinations and surgical procedures. The four clinical project partners will collect these data sets. “We're not just gathering data that’s already available; we can adapt the data collection specifically to our needs,” says Meybohm.“We hope that this will increase the relevance and accuracy of the algorithms and recommended actions.”
Trust built upon transparent operation
A great challenge in developing the CDS system is its usability. “We have to design the AI-based solution so that enhances physicians’ work and is not seen as a burden,” emphasizes Hennemuth, who also holds a professorship at the Charité – Universitätsmedizin Berlin. “The essential trust in new technology can only happen if we clearly present how and with what certainty the algorithms come to their results.” The AI should not act as a black box: it should make uncertainties and possible sources of error transparent. Development will feature close coordination with the project’s clinical partners and an ethics team at RWTH Aachen University.
In the long term, the CDS system could even provide another benefit: It might be able to detect previously unidentified data relationships between input information and frequency of complication. This could help unearth previously unknown risk factors. These results could be integrated into upcoming guidelines and help make operations even safer. The economic impact and possible new opportunities for healthcare are also being investigated in the project: model calculations are being performed by the Technical University of Munich.
KIPeriOP
is a research project funded by the German Federal Ministry of Health with 1.5 million euros until September 2023. It aims to improve perioperative risk management and decrease perioperative mortality and permanent damage. The interdisciplinary consortium is coordinated by the University Hospital of Würzburg and Fraunhofer MEVIS. Physicians from University Hospital of Würzburg (Dr. J. Stumpner, Dr. P. Bendz, Dr. A. Englert), Asklepios Medical School GmbH (Prof. Dr. A. Ghanem), Frankfurt University Hospital (Prof. Dr. Dr. K. Zacharowski, Dr. P. Booms), and Charité – Universitätsmedizin Berlin (Prof. Dr. C. Spies, Prof. Dr. F. Balzer) perform patient treatment, implementation research, development and enhancement of machine-readable protocols, and real-time validation. Fraunhofer MEVIS (Dr. M. Westphal, M. Hüllebrand, S. Archipovas) is responsible for developing and evaluating innovative and accessible AI modules for clinical decision support. Börm Bruckmeier Verlag (N. Blanck, Dr. P. Börm) is responsible for CDS development and product approval. The research topic of applied ethics at RWTH Aachen University (Prof. Dr. S. Nagel) is analyzing and designing the ethical requirements for digital clinical decision support. The Department of Sports and Health Sciences at the Technical University of Munich (Prof. Dr. L. Sundmacher, A. Flothow) is investigating economic effects of clinical decision support.
Material
Related Topics
 Fraunhofer Institute for Digital Medicine MEVIS
Fraunhofer Institute for Digital Medicine MEVIS